Iron Overload and Liver Health: Understanding the Connection
Receiving a diagnosis of hemochromatosis can be a daunting experience. You’ve likely been told that your body is holding onto too much iron, and perhaps the connection to your liver has been mentioned. It’s natural to feel a mix of fear and confusion when faced with a new health condition, especially one that sounds as serious as iron overload.
But take a deep breath. This article is designed to provide you with clear, comprehensive information about hemochromatosis, its link to liver disease, and what you can do to help address your condition. Our goal is to empower you with knowledge, alleviate some of your anxieties, and guide you on your journey toward living well with hemochromatosis.
What is Hereditary Hemochromatosis?
At its core, hemochromatosis is a genetic disorder that causes your body to absorb too much iron from the food you eat. Iron is an essential mineral, vital for many bodily functions, including carrying oxygen in your blood. However, like many good things, too much iron can be harmful. In hemochromatosis, this excess iron doesn’t get excreted; instead, it may accumulate in various organs, potentially leading to damage over time. The liver is a primary target for this iron buildup, but other organs such as the heart, pancreas, joints, and pituitary gland can also be affected.
There are different types of hemochromatosis, but the most common form is hereditary hemochromatosis (HH), also known as primary hemochromatosis. This type is caused by mutations in genes, most commonly the HFE gene. If you have HH, it means you’ve inherited a gene variation from one or both of your parents. It’s important to understand that while you may have inherited the genetic predisposition, not everyone with the gene mutations will develop significant iron overload or symptoms.
In This Article:
The Liver: A Central Player in Iron Overload
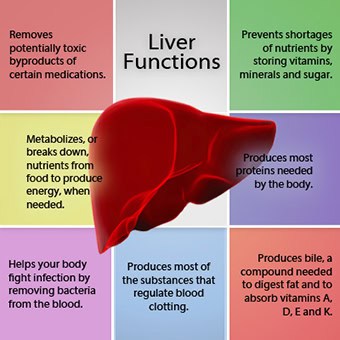
The liver is a remarkable organ, performing over 500 vital functions, including filtering toxins, producing proteins and hormones, as well as storing vitamins and minerals. It plays a central role in iron metabolism, acting as the primary storage site for excess iron in the body. This is why the liver is often the first and most significantly impacted organ in individuals with hemochromatosis.
When iron accumulates in the liver, it can lead to a range of problems, from mild inflammation to severe, life-threatening conditions. The excess iron acts as a pro-oxidant, meaning it can create harmful free radicals that damage liver cells. This damage can trigger a cascade of events:
- Inflammation: The initial response to iron overload in the liver is often inflammation.
- Fibrosis: If the inflammation persists, the liver attempts to repair itself by forming scar tissue, a process called fibrosis. Think of it like a scar on your skin; while it helps to heal, too much scar tissue can impair the organ’s function.
- Cirrhosis: With continued iron accumulation and progressive fibrosis, the scar tissue can become widespread and disrupt the liver’s normal structure, leading to cirrhosis. Cirrhosis is a serious condition where the liver’s ability to function is severely compromised. It can lead to liver failure, a life-threatening condition where the liver can no longer perform its essential tasks.
- Hepatocellular Carcinoma (Liver Cancer): Cirrhosis is a major risk factor for developing liver cancer. The chronic inflammation and cell damage caused by iron overload, if left unchecked, can increase the likelihood of cancerous cell growth in the liver.
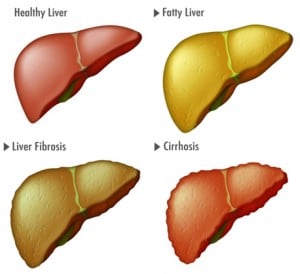
Understanding this progression is crucial, but it’s equally important to know that this process may take years or even decades, and that early diagnosis and treatment can prevent, significantly slow down, or possibly even reverse the development of these severe liver complications.
Recognizing the Signs & Symptoms of Hemochromatosis
One of the challenges with hemochromatosis is that its early symptoms can be vague, non-specific, and often mimic those of other common conditions. Many people don’t experience symptoms until significant iron overload has occurred, sometimes many years after the iron accumulation began. This is why hemochromatosis is often called a “silent disease.”
When symptoms do appear, they can vary widely from person to person and often depend on which organs are most affected. Common symptoms include:
General Symptoms:
- Fatigue and Weakness: This is one of the most common and often earliest symptoms, but it’s also very non-specific.
- Joint Pain: Often affecting the knuckles of the fingers, wrists, knees, hips, and/or ankles. If this progresses to arthritis, this is often referred to as “hemochromatosis arthropathy.”
- Abdominal Pain: Especially in the upper right quadrant, where the liver is located.
- Loss of Libido (Sex Drive) and Erectile Dysfunction: Iron accumulation in the pituitary gland or testes can disrupt hormone production.
- Skin Pigmentation Changes: A bronze or grayish discoloration of the skin, sometimes referred to as “bronze diabetes.” This is due to iron deposits in the skin.
Liver-Related Symptoms (Indicating More Advanced Disease):
- Enlarged Liver (Hepatomegaly): Your doctor may detect this during a physical examination.
- Jaundice: Yellowing of the skin and eyes, indicating severe liver dysfunction.
- Ascites: Swelling in the abdomen due to fluid buildup, a sign of advanced liver disease.
- Edema: Swelling in the legs and ankles.
- Spider Angiomas: Small, spider-like blood vessels on the skin.
Other Organ-Specific Symptoms:
- Heart Problems: Shortness of breath, chest pain, irregular heartbeats (arrhythmias), or even heart failure due to iron buildup in the heart muscle.
- Diabetes: Iron accumulation in the pancreas can damage insulin-producing cells, potentially contributing to “bronze diabetes” skin pigmentation changes mentioned above.
- Hypothyroidism: Iron deposits in the thyroid gland can impair its function.
It’s important to reiterate that these symptoms can also be caused by many other conditions. If you are experiencing any of these, it’s crucial to discuss them with your doctor.
The Path to Diagnosis: How Hemochromatosis is Identified
Given the non-specific nature of symptoms, hemochromatosis is often diagnosed through routine blood tests or when investigating other health concerns. The diagnostic process typically involves a combination of blood tests, genetic testing, and sometimes imaging studies or (rarely) a liver biopsy.
Common Steps in the Path to Diagnosing Hemochromatosis
1. Blood Tests: The First Clues
Several blood tests are crucial for identifying iron overload:
- Serum Ferritin: Ferritin is a protein that stores iron in your body. A high serum ferritin level is a strong indicator of excess iron. However, ferritin can also be elevated due to inflammation, infection, or other liver conditions, so it’s not solely diagnostic.
- Transferrin Saturation (TSAT): Transferrin is a protein that transports iron in the blood. TSAT measures how much iron is bound to transferrin. A high TSAT (typically >55% in men and postmenopausal women, and >50% in premenopausal women) is often the earliest indicator of iron overload, even before ferritin levels rise significantly. It reflects the amount of iron readily available to be deposited in tissues.
- Serum Iron: This measures the amount of iron circulating in your blood. While useful, it can fluctuate throughout the day and is usually interpreted in conjunction with transferrin saturation and ferritin.
If these blood tests suggest iron overload, your doctor may recommend genetic testing.
2. Genetic Testing: Confirming the Predisposition
Genetic testing is a more specific way to diagnose hereditary hemochromatosis. It involves a simple test to look for variations in the HFE gene, specifically the C282Y and H63D mutations.
- C282Y/C282Y: If you have two copies of the C282Y gene variation (one from each parent), you are homozygous for this mutation. This is the most common genotype associated with significant iron overload and is highly predictive of hereditary hemochromatosis.
- C282Y/H63D: If you have one copy of the C282Y mutation and one copy of the H63D mutation (compound heterozygous), you are at a lower risk of severe iron overload compared to C282Y/C282Y, but iron accumulation can still occur.
- H63D/H63D: Two copies of the H63D variation are generally not associated with significant iron overload, however individual expression of these genes may contribute to high iron and ferritin levels.
- Other Genes: While HFE gene mutations are responsible for the vast majority of hereditary hemochromatosis cases, mutations in other genes (such as HJV, HAMP, TFR2, and SLC40A1) can cause rarer forms of hemochromatosis.
3. Imaging Studies:
Once iron overload is suspected, imaging studies can help assess the extent of iron deposition, particularly in the liver:
- MRI (Magnetic Resonance Imaging): Specialized MRI techniques, such as T2*-weighted MRI, can directly measure the amount of iron in the liver and other organs non-invasively. This has largely replaced the need for liver biopsies in many cases.
- Elastography (FibroScan): This non-invasive test measures liver stiffness, which can indicate the presence and severity of fibrosis or cirrhosis.
4. Liver Biopsy (Less Common Now):
In the past, a liver biopsy (a procedure where a small sample of liver tissue is removed and examined under a microscope) was often performed to confirm the diagnosis and assess the extent of liver damage and iron concentration. While still sometimes used, particularly if there’s uncertainty about the diagnosis or a need to rule out other liver diseases, advanced MRI techniques have significantly reduced the necessity of this invasive procedure.
Conventional Treatment Options: Releasing the Iron
The good news is that hemochromatosis is a treatable condition, especially when diagnosed early. The primary goal of treatment is to reduce the body’s iron stores to healthy levels and then maintain them there.
Phlebotomy (Therapeutic Blood Removal): The Cornerstone of Treatment
Phlebotomy, also known as venesection or therapeutic bloodletting, is the most effective and widely used treatment for hereditary hemochromatosis. It’s essentially the same process as donating blood. By regularly removing blood, your body is forced to use its iron stores to make new red blood cells, thereby gradually reducing the excess iron.
The phlebotomy regimen is tailored to each individual:
- Induction Phase: Initially, phlebotomies may be performed frequently until your iron levels (specifically ferritin and transferrin saturation) fall within the normal range. The frequency depends on the severity of your iron overload. During this phase, you may feel a bit tired after treatments, but this usually improves as your iron levels normalize.
- Maintenance Phase: Once your iron levels are normalized, the frequency of phlebotomies will be reduced to prevent iron re-accumulation. This phase may continue for life, if required. Regular blood tests will be conducted to monitor your iron levels and adjust the phlebotomy schedule as needed.
Phlebotomy is a safe and generally well-tolerated procedure. The main side effects are usually minor, such as temporary fatigue, lightheadedness, or bruising at the needle site. It’s crucial to stay well-hydrated before and after your phlebotomy appointments.
Chelation Therapy (Less Common for HH):
Chelation therapy involves taking medications (either orally or intravenously) that bind to iron in the blood and help the body excrete it. This treatment is generally reserved for individuals who cannot undergo phlebotomy, such as those with severe anemia, certain heart conditions, or rare forms of hemochromatosis where phlebotomy is not effective. Examples of chelating agents include deferoxamine, deferasirox, and deferiprone. These medications can have more significant side effects than phlebotomy and require careful monitoring – thus why this form of treatment is not recommended frequently.
Management of Complications:
In addition to iron reduction, managing any complications arising from hemochromatosis is crucial and should be tailored to the individual:
- Liver Disease: Regular monitoring of liver function tests and imaging studies is essential. If cirrhosis or liver cancer develops, specialized medical and potentially surgical interventions will be necessary, including surveillance for hepatocellular carcinoma.
- Diabetes: Management with diet, exercise, and medication as recommended by your physician.
- Heart Conditions: Medications and other treatments for arrhythmias, heart failure, or other cardiac issues.
- Joint Pain: Pain relievers, anti-inflammatory medications, and physical therapy.
Living Well with Hemochromatosis: Nutritional Considerations and Natural Remedies
While phlebotomy is the cornerstone of treatment, lifestyle modifications, particularly regarding diet, can play a supportive role. It’s important to emphasize that these are complementary strategies and should never replace conventional medical treatment. Always discuss any dietary changes or supplements with your doctor.
Natural Approaches That May Provide Support to Liver Health
Dietary Considerations:
The goal of dietary modifications in hemochromatosis is not to completely eliminate iron (which is impossible and unhealthy) but to minimize the absorption of iron from your diet and avoid foods that significantly contribute to iron overload.
- Limit High-Iron Foods (in Moderation): While you may not need to completely avoid iron-rich foods, it’s wise to consume them in moderation, especially red meat, organ meats (like liver), and iron-fortified cereals and breads. The type of iron found in animal products (heme iron) is absorbed more readily than iron from plant sources (non-heme iron).
- Read more here: Heme vs Non-Heme Iron in Hemochromatosis
- Avoid Raw Shellfish: Raw oysters, clams, and mussels can contain Vibrio vulnificus, a bacterium that thrives in iron-rich environments. Individuals with significant hemochromatosis are at a higher risk of severe, life-threatening infections from this bacterium. Always cook shellfish thoroughly.
- Be Mindful of Vitamin C: Vitamin C (ascorbic acid) enhances the absorption of non-heme iron. While a healthy diet should include Vitamin C, it’s generally recommended to avoid taking large doses of Vitamin C supplements, especially with meals rich in iron. Small amounts of Vitamin C from fruits and vegetables are usually not a concern.
- Limit Alcohol: Alcohol, particularly heavy consumption, can significantly increase the risk of liver damage and accelerate the progression of liver disease in individuals with hemochromatosis. It’s advisable to limit or avoid alcohol entirely, especially if you have existing liver damage.
- Foods that Inhibit Iron Absorption:
- Tea and Coffee: Tannins in tea and coffee can inhibit iron absorption. Drinking tea or coffee with meals may reduce iron uptake.
- Calcium: Calcium can interfere with iron absorption. Consuming calcium-rich foods (dairy products, fortified plant milks) with meals might have an inhibitory effect, specifically on heme iron foods.
- Phytates: Found in legumes, whole grains, and seeds, phytates can also inhibit iron absorption. Soaking and sprouting grains and legumes can reduce phytate levels.
- Oxalates: Present in spinach, rhubarb, and beet greens, oxalates can bind to iron and reduce its absorption.
- For the most comprehensive view of foods to inhibit iron absorption, Dr. Kristina Lewis has written Cooking for Hemochromatosis – an excellent resource and cookbook!
Nutritional Supplements and Natural Remedies (Use with Caution and Doctor’s Approval):
The role of nutritional supplements and natural remedies in managing hemochromatosis is supportive and adjunctive only. They do not replace phlebotomy or other conventional treatments. Always consult your doctor before taking any supplements, as some can be harmful or interfere with your treatment.
- Milk Thistle (Silymarin): Milk thistle is a popular herbal supplement often used for liver support. Some studies suggest it may have antioxidant and anti-inflammatory properties that could be beneficial for liver health.
- Curcumin (Turmeric): Curcumin, the active compound in turmeric, has strong anti-inflammatory and antioxidant properties. Clinical research suggests it might have iron-chelating effects, as well as significant ferritin and transferrin saturation lowering abilities.
- Green Tea Extract: Green tea contains compounds called catechins, which have antioxidant properties and have been shown in some studies to chelate iron.
- Calcium: As mentioned in dietary considerations, calcium can inhibit heme iron absorption.
- For the most complete, yet easy to understand, book detailing nutritional supplements and natural remedies to reduce iron levels, Dr. Eric Lewis has written Holistic Help for Hemochromatosis.
Important Considerations for Supplements:
- Avoid Iron-Containing Supplements: This might seem obvious, but always check labels carefully. Many multivitamin supplements contain iron, which you must avoid.
- Be Skeptical of “Miracle Cures”: There are no natural remedies or supplements that can cure hemochromatosis or effectively remove excess iron from your body like phlebotomy can. Be wary of claims that promise otherwise.
- Quality and Purity: If you do choose to take a supplement, ensure it’s from a reputable manufacturer and has been tested for purity and potency.
- Interactions: Supplements can interact with medications, including those for other conditions you may have. Always inform your doctor about all supplements you are taking.
The Emotional Landscape: Coping with a Diagnosis
It’s entirely normal to feel a range of emotions after a hemochromatosis diagnosis – fear, anger, sadness, or even relief at finally having an answer to nagging symptoms. Remember, you are not alone.
- Educate Yourself: The more you understand your condition, the less frightening it becomes. This article is a starting point; continue to read reliable sources and ask your medical team questions.
- Build a Support System: Talk to trusted family members and friends about what you’re going through. Connecting with others can be incredibly validating and provide practical advice.
- Communicate with Your Healthcare Team: Maintain open and honest communication with your doctors. Don’t hesitate to ask questions, express your concerns, and seek clarification on anything you don’t understand. Your healthcare team is there to support you.
- Prioritize Self-Care: Manage stress through activities you enjoy, get adequate sleep, and incorporate exercise into your routine (as advised by your doctor). Taking care of your overall well-being is crucial when managing a chronic condition.
Looking Ahead: A Positive Outlook
While hemochromatosis is a lifelong condition, it is a highly manageable one. With early diagnosis and consistent treatment, most individuals with hemochromatosis can live long, healthy lives with a normal life expectancy. Regular phlebotomies effectively remove excess iron, prevent organ damage, and can often reverse early symptoms.
Your diagnosis is not a life sentence; it’s a call to action. By taking an active role in your care, adhering to your treatment plan, and making informed lifestyle choices, you can effectively manage your hemochromatosis and protect your liver and overall health. Embrace the knowledge you gain, lean on your support system, and look forward to a future where hemochromatosis is a condition you manage, not one that defines you.
This article aims to provide a comprehensive overview for newly diagnosed individuals. However, it is not a substitute for professional medical advice. Always consult with your doctor or healthcare provider for personalized diagnosis, treatment, and management of hemochromatosis.
Top Six Ways to Take Charge of Your Health with Iron Overload
Hemochromatosis can be scary, lonely, and intimidating.
As naturopathic doctors and a family personally impacted by hereditary hemochromatosis, we want to empower people with iron overload to take charge and learn how to live healthier lives with hemochromatosis.
How We Can Help
Here are six things you can do right now to take charge of your health with iron overload:
- If you haven’t already, be sure to sign up for our newsletter that contains great info on a wide range of subjects related to iron overload.
- To learn more about hemochromatosis, be sure to check out our Hemochromatosis Learning Center on our website, with links to a wide range of topics such as symptoms, treatments, genetics, as well as diet and nutritional information relating to iron overload.
- My book Holistic Help for Hemochromatosis is a complete guide to the use of diet and supplements in healing from iron overload. Available as a paperback and also as an instant-download e-book.
- My wife’s cookbook Cooking for Hemochromatosis is a comprehensive guidebook to help you plan, shop, and cook to reduce iron in your diet. Much more than just a cookbook, it will teach you how to decide what to eat, plan meals, and enjoy food again when facing iron overload.
- We have created a line of nutritional supplements designed to help support the health of an individual with high iron.
- We have also created the only online video course in the world designed for patients with hemochromatosis. 25 videos to help you understand your condition are packed into 5 modules and 1 bonus module.
https://www.mayoclinic.org/diseases-conditions/hemochromatosis/symptoms-causes/syc-20351443
https://medlineplus.gov/ency/article/002422.htm
https://www.nhs.uk/conditions/vitamins-and-minerals/iron/
https://academic.oup.com/jes/article/6/Supplement_1/A317/6788787
https://www.mayoclinic.org/diseases-conditions/hemochromatosis/symptoms-causes/syc-20351443
https://www.nhs.uk/conditions/haemochromatosis/causes/
https://www.ncbi.nlm.nih.gov/books/NBK430862/
https://www.michiganmedicine.org/health-lab/what-does-liver-do-and-how-do-i-keep-mine-healthy
https://my.clevelandclinic.org/health/diseases/14971-hemochromatosis-iron-overload
https://pmc.ncbi.nlm.nih.gov/articles/PMC5537786/
https://www.nhs.uk/conditions/cirrhosis/
https://www.mayoclinic.org/diseases-conditions/hemochromatosis/symptoms-causes/syc-20351443
https://www.mayoclinic.org/diseases-conditions/hepatocellular-carcinoma/cdc-20354552
https://www.cdc.gov/hereditary-hemochromatosis/about/index.html
https://www.mayoclinic.org/diseases-conditions/liver-problems/symptoms-causes/syc-20374502
https://www.ucsfhealth.org/medical-tests/serum-iron-test
https://www.haemochromatosis.org.uk/h63d-h63d-homozygous
https://pubs.rsna.org/doi/full/10.1148/radiol.221856